Table of Contents
I. How does the Stomach Function?
II. What is a Gastrointestinal Motility Disorder?
III. Understanding Gastroparesis
IV. Difference Between Gastroparesis & GERD
V. Type 2 Diabetes & Gastroparesis
VII. Treating Gastric Motility Disorders
How does the Stomach Function?
The stomach is a complicated organ that is responsible for many important bodily functions. The food travels down the windpipe and enters the stomach through a muscular valve called the esophageal sphincter. The stomach secretes enzymes that help digest the food we eat. Once the food is broken down, muscle tissue called rugae contract and churn the food to assist digestion. If one of these functions is not working, several complications can occur.
If the stomach is unable to churn this food through the digestive tract, you may experience a gastrointestinal (GI) motility disorder. These disorders may include GI problems like gastroparesis and chronic constipation. These conditions can be treated with medications like Reglan (metoclopramide), Motegrity (prucalopride), and Motilium (domperidone). [1]
Gastrointestinal motility disorders can cause several digestive symptoms that may make everyday life difficult. These issues may lead to symptoms like gas, severe constipation, abdominal pain, vomiting, and bloating. GI motility disorders may occur due to a problem with the muscle that controls peristalsis. Peristalsis is the involuntary constriction and relaxation of the intestinal muscles. Peristalsis creates wavelike movements that push the stomach contents along with the digestive system.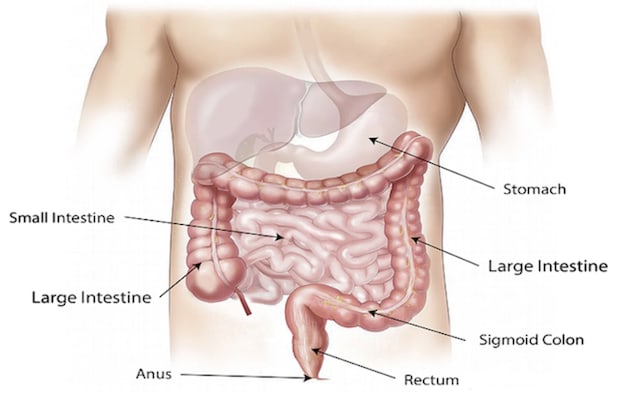
What is a Gastrointestinal Motility Disorder?
Get savings updates for Reglan
Motility disorders may also occur due to problems with the nerves or hormones that tell the muscles to perform peristalsis. These nerve problems can happen for several reasons and are common in type 2 diabetes patients. [2]
Understanding Gastroparesis
Gastroparesis is one such motility disorder that occurs when nerves are damaged or stop working. The main nerve is called the vagus nerve, which is vital in controlling food movement through the stomach. When this nerve is damaged, the intestinal muscles are not working correctly, and the movement of food through the digestive system may slow or stop altogether. This is why gastroparesis is also known as delayed gastric emptying. [3]
a. Symptoms of Gastroparesis
If you are experiencing gastrointestinal problems, you may want to record your symptoms to assist in your diagnosis. Many GI problems have similar symptoms, but those with gastroparesis may experience:
- Abdominal pain
- Weight loss
- Malnutrition
- Vomiting undigested food a few hours after eating
- Nausea
- Abdominal bloating [4]
Gastrointestinal disorders often have similar symptoms, which can make diagnosis difficult. Symptoms of gastroparesis most often mirror another GI disorder called GERD (gastroesophageal reflux disease). The main difference between the two conditions involves the area of the stomach where problems occur. In GERD, issues may arise when chronic acid reflux weakens the lower esophageal sphincter (LES). The LES separates the esophagus from the stomach. The LES must remain strong and closed; otherwise, stomach acid may cause backflow into the esophagus and lead to unpleasant acid reflux symptoms. These symptoms may include: The other big difference between GERD and gastroparesis is the cause. These conditions may occur for several reasons, but GERD is more related to diet than gastroparesis. Eating spicy foods, acidic foods or drinks, and greasy food can lead to acid reflux symptoms. Gastroparesis pain also occurs in the lower gastrointestinal region, whereas GERD occurs in the upper stomach and esophagus. [5] As mentioned above, damage to the vagus nerve is one main cause of gastroparesis. Gastroparesis may occur for other reasons, but vagus nerve damage is a significant risk factor because it is integral to the gastrointestinal system's function. When the vagus nerve is not working properly, it may not send signals to the stomach muscles telling it to contract and propel food through the intestines. [4] Type 2 diabetes is one common cause of vagus nerve damage. Type 2 diabetes is a chronic condition that affects the way the body metabolizes glucose (sugar). Glucose is an essential fuel source for the body, and when this fuel cannot move into cells, insulin may be needed to maintain glucose levels. [6] Researchers have found that gastroparesis occurs more commonly in those with high or uncontrolled blood glucose levels. Some type 2 diabetes patients may experience uncontrolled blood sugar for long periods, putting them at risk of gastroparesis. High blood sugar damages the blood vessels that supply nerves and organs vital oxygen and nutrition. If the vagus nerve does not receive the proper nutrition, gastroparesis may occur. Many people with type 2 diabetes may not realize they have gastroparesis until they experience severe symptoms like chronic constipation or vomiting. [7] Several tests will be performed to determine gastroparesis. You will likely undergo gastric emptying tests to see how fast your stomach empties its contents. An endoscopy may be performed as well. These tests include: Scintigraphy: You will eat a light meal like eggs and toast, but a small amount of radioactive material will be within your meal. Once you eat your food, this radioactive material will travel into the stomach. Your doctor will place a scanner over your abdomen and monitor the rate at which food leaves your stomach. Upper Gastrointestinal Endoscopy: This procedure involves examining your upper digestive system. A tiny camera on the end of a flexible tube is inserted down into the stomach to diagnose conditions like peptic ulcers or pyloric stenosis. These conditions have similar symptoms to gastroparesis so that they will be ruled out before a diagnosis. [4] The goal of treatment for gastric motility is to treat underlying problems and symptoms. If diabetes is a contributing factor to your gastroparesis, it is essential to make sure your blood sugar levels remain at a healthy level. Patients can manage many gastroparesis symptoms with diet changes, including: Along with diet changes, several medications like Reglan (metoclopramide), Motegrity (prucalopride), and Motilium (domperidone) can be used to aid in treatment. Motegrity is used for constipation that lasts for three months and has no known cause. Reglan is targeted towards GERD symptoms, like healing the ulcers and sores in the esophagus. Lastly, Motilium increases the movements or contractions of the stomach and bowel. Your doctor will decide which medication is right for your gastric motility disorder. [8] If your gastroparesis is severe, it may also require surgery or feeding tubes. Some with gastroparesis may be unable to tolerate food or liquids, which may require you to consume nutrients through a feeding tube passed through your mouth into your small intestine. Talk to your doctor if you are experiencing severe stomach problems. [4] The content in this article is intended for informational purposes only. This website does not provide medical advice. In all circumstances, you should always seek the advice of your physician and/or other qualified health professionals(s) for drug, medical condition, or treatment advice. The content provided on this website is not a substitute for professional medical advice, diagnosis, or treatment.
Difference between Gastroparesis & GERD
Type 2 Diabetes & Gastroparesis

Diagnosing Gastroparesis
Treating Gastric Motility Disorders
